BPCI-A Changes: What They Mean for Providers and Health Systems
Managing financial risk while delivering high-quality care is a challenge for ACOs, hospitals, and payers. This guide explores how Bundled Payments for Care Improvement (BPCI) and BPCI Advanced enhance efficiency, reduce costs, and improve outcomes. Download our free comparison PDF to see the key differences between the models and how your organization can benefit.
February 8, 2025
9 min. read

Bundled Payments for Care Improvement (BPCI) is transforming how healthcare organizations manage costs and improve patient care by shifting from traditional fee-for-service models to bundled, episode-based reimbursement. For risk-bearing entities such as accountable care organizations (ACOs) and managed care organizations, ensuring high-quality, coordinated care while controlling spending is a top priority. Many conditions—from cardiac and orthopedic procedures to chronic disease management—require complex, multi-provider treatment, often leading to care fragmentation and cost variability.
The BPCI initiative offers a structured, value-based approach that aligns financial incentives with care quality, encouraging greater provider collaboration and cost-effective care delivery. By replacing volume-based payments with a bundled model, healthcare organizations can improve patient outcomes, streamline care coordination, and reduce unnecessary spending.
What is BPCI?
Traditionally, healthcare reimbursement has been based on a fee-for-service model, where providers are compensated for each service delivered. While this model ensures that care is readily available, it can sometimes lead to uncoordinated treatment, variable costs, and inconsistent patient outcomes.
To address these challenges, the Centers for Medicare & Medicaid Services (CMS) introduced the Bundled Payments for Care Improvement (BPCI) initiative to align provider incentives, enhance care coordination, and promote cost-effective treatment approaches. Instead of separate payments for each service, BPCI bundles reimbursement for an entire episode of care, encouraging collaboration among providers and a stronger focus on quality and efficiency.1
BPCI models
The BPCI initiative was initially structured around four payment models, each testing different bundled payment approaches across acute and post-acute care settings:1
Model 1: Covered only inpatient hospital stays, with hospitals receiving a discounted payment rate from Medicare while physicians were paid separately.
Models 2, 3, and 4: Expanded coverage beyond hospital stays to include post-acute care, skilled nursing, rehabilitation, and home health services. These models introduced financial risk-sharing across broader care episodes.
In September 2018, CMS phased out Models 2, 3, and 4, shifting to a more streamlined and risk-adjusted approach with BPCI Advanced, which we will explore in the next section, detailing how it expands upon previous models with enhanced risk-sharing, outpatient care integration, and mandatory quality tracking.
BPCI Advanced: The next phase of value-based care
What is BPCI Advanced?
Building upon the original BPCI models, BPCI Advanced (BPCI-A) enhances financial risk management, provider incentives, and care coordination. One of its most significant improvements is its qualification as an Advanced Alternative Payment Model (Advanced APM) under MACRA, allowing providers to earn bonus payments for meeting quality and cost-efficiency benchmarks.
Unlike traditional models, BPCI Advanced requires participating providers to actively coordinate care across settings—ensuring that hospitals, outpatient specialists, and primary care physicians communicate effectively. Many patients receive care from providers who may not have full access to their medical history, leading to fragmented treatment and gaps in follow-up care. By promoting greater provider collaboration, BPCI Advanced streamlines care, improves patient outcomes, and reduces preventable hospitalizations and emergency department visits.2
Key features of BPCI Advanced
To succeed under BPCI Advanced, organizations must understand and leverage its core features, which are structured to drive financial sustainability, streamline care delivery, and reward high-quality performance:2
Allows voluntary participation, enabling organizations to join based on readiness and alignment with value-based care strategies.
Holds participants financially accountable through a single retrospective bundled payment and one risk track over a 90-day clinical episode.
Expands episode coverage to 29 inpatient and three outpatient clinical episodes, organized into eight Clinical Episode Service Line Groups (CESLGs), with two additional multi-setting categories.
Qualifies participants for Advanced APM status under MACRA, allowing eligible providers to earn bonus payments tied to performance.
Ties payments to quality measures, requiring participants to report and meet performance benchmarks to optimize reimbursement.
Provides preliminary target prices prior to each model year and finalizes pricing during reconciliation based on patient mix and care trends.
BPCI vs. BPCI Advanced: Key differences
BPCI Advanced presents a more structured and data-driven model, making it an effective tool for organizations assuming financial risk. Specifically, accountable care organizations, managed care organizations and payers, as well as hospitals and health systems stand to benefit from the program’s improvements in financial predictability, quality tracking, and cost efficiency.
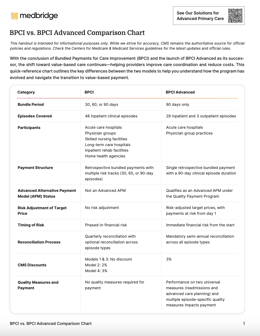
To help you better understand the differences between BPCI and BPCI Advanced, we’ve prepared a detailed comparison chart outlining key changes in eligibility, payment structures, and quality requirements based on CMS's official program guidelines. Download the free BPCI vs. BPCI-A Comparison Chart PDF below to explore how BPCI-A aligns with your organization's value-based care strategy.
BPCI vs. BPCI Advanced Comparison Chart PDF
Fill out the form to unlock your free PDF!
What do these differences mean?
BPCI-A offers stronger financial predictability and quality incentives than the original BPCI models. By expanding outpatient episode coverage, requiring mandatory quality reporting, and introducing risk-adjusted pricing, the program better aligns with value-based care initiatives.
These enhancements allow:
ACOs to integrate BPCI-A episodes into their risk-based strategy, improving efficiency and patient outcomes.
Managed care organizations and payers to align their Medicare Advantage plans with bundled payment models, optimizing cost and quality management.
Hospitals and health systems to reduce readmissions, streamline care pathways, and lower Medicare spending through better care coordination.
BPCI-A’s structure enables these organizations to manage financial risk more effectively while ensuring consistent, high-quality care delivery across provider networks.
Challenges in BPCI Advanced and how to solve them
While BPCI Advanced provides a structured framework for cost control and quality improvement, its success depends on proactively managing key challenges. Below are the biggest hurdles ACOs, hospitals, and managed care organizations face—and strategies to overcome them.
1. Managing financial risk
Bundled payments help control overall healthcare spending, but unexpected high-cost cases or variability in patient needs can make it challenging to stay within target price limits. Without careful cost management, hospitals and ACOs risk financial penalties.
Strategies to overcome it:
Use risk-adjusted pricing models to account for patient complexity and ensure fair reimbursement.
Leverage claims data and predictive analytics to track spending trends and anticipate high-cost cases.
Identify cost inefficiencies in care delivery and implement strategies to contain excess spending.
2. Standardizing care across providers
BPCI Advanced requires consistent, evidence-based care across multiple providers. However, variability in practice patterns can lead to inconsistent costs and quality, making it difficult for ACOs, hospitals, and payers to achieve program goals.
Strategies to overcome it:
Develop standardized clinical pathways to align providers with evidence-based treatment protocols.
Implement integrated communication tools to ensure seamless coordination across care teams.
Provide continuing education and engagement to reinforce best practices and treatment guidelines.
For hospitals, ACOs, and payers looking to standardize care and manage costs, Medbridge’s white-labeled digital MSK solution offers a scalable and cost-effective way to enhance care coordination, member engagement, and financial sustainability within a bundled payment structure. By integrating customized care plans, real-time patient progress tracking, and digital engagement tools, organizations can improve patient outcomes while keeping care within their network. This approach not only reduces unnecessary utilization but also creates new revenue opportunities by delivering high-quality, accessible care at scale.
3. Provider engagement and alignment
For BPCI Advanced to succeed, providers must fully understand and buy into the model. Misalignment in financial incentives or lack of familiarity with bundled payments can create resistance.
Strategies to overcome it:
Educate providers on how bundled payments impact reimbursement, workflows, and patient care.
Align financial incentives by tying compensation to cost efficiency and quality benchmarks.
Encourage collaboration among care teams by fostering shared decision-making and performance tracking.
4. Optimizing post-acute and outpatient care
Many cost inefficiencies occur after hospital discharge, particularly when post-acute care decisions are inconsistent. Without proper coordination, hospitals and ACOs may see unnecessary readmissions and increased post-acute spending.
Strategies to overcome it:
Expand outpatient rehabilitation and therapy programs to prevent avoidable hospitalizations and readmissions.
Use early intervention strategies to proactively identify high-risk patients and provide timely care.
Strengthen care transitions between inpatient and post-acute providers to improve continuity of care.
How BPCI supports value-based care organizations
Managing financial risk while ensuring high-quality patient care is a constant challenge for accountable care organizations, managed care organizations, and hospitals. Traditional payment models can lead to unpredictable costs, fragmented care coordination, and inconsistent patient outcomes, making it difficult for organizations to control spending without compromising care quality. The Bundled Payments for Care Improvement initiative offers a structured solution that aligns financial incentives with efficient, evidence-based care delivery.
By replacing volume-driven fee-for-service payments with episode-based reimbursement, bundled payments shift the focus toward value and efficiency. Providers are encouraged to deliver coordinated, cost-effective care across the entire treatment episode, from initial diagnosis to recovery. This approach enables greater financial predictability, fewer unnecessary interventions, and stronger care integration across provider networks.
As value-based care continues gaining traction, organizations must adopt scalable strategies that drive both financial and clinical success. Those that leverage data-driven decision-making, standardized care pathways, and provider engagement initiatives will be best positioned to optimize cost savings while maintaining high-quality outcomes under BPCI Advanced.
BPCI Advanced and the future of value-based care
BPCI Advanced offers a structured, data-driven model that helps ACOs, hospitals, and managed care organizations optimize cost control, care coordination, and patient outcomes. By aligning financial incentives with quality and efficiency, the model empowers organizations to reduce unnecessary costs while delivering better care. However, long-term success depends on strategic financial planning, provider engagement, and scalable care pathways that drive measurable results.
As value-based care continues evolving, organizations that invest in standardized, technology-driven solutions will be best positioned for long-term sustainability and growth. By leveraging data analytics, provider collaboration, and digital care platforms, healthcare leaders can enhance patient experiences, improve financial outcomes, and strengthen network integration.
For population-level care strategies that extend beyond episodes, CMS’s ACO REACH model offers an aligned approach focused on health equity, access, and long-term outcomes.
It’s worth noting the upcoming TEAM Model, a mandatory episode-based payment model focused on surgical care. While BPCI-A offers flexibility through voluntary participation, the TEAM Model introduces required participation and expanded integration with primary care. Learn how the TEAM Model builds on BPCI-A and what it means for hospitals and ACOs.
References





